At a time of unprecedented support for Medicare for All, half-measure proposals are being floated by members of Congress and Presidential candidates. The chief beneficiaries of these proposals are for-profit insurance and pharmaceutical corporations. Not surprisingly, virtually all of those who are making these proposals receive funding from those very corporations.
Is there anything wrong with that? After all, the ultimate goal for healthcare reform is to ensure universal coverage, not to take down a particular industry. And passing any of these compromise proposals into law would undoubtedly be an easier lift politically than Medicare for All.
Yet half-measures like a “public option” or “just expand the Affordable Care Act” leave undisturbed the core problem of the U.S. healthcare system: the massive hole draining our taxpayer healthcare dollars to the benefit of corporations which prioritize profits over care. If we don’t plug that profiteering hole, we don’t fix the problem.
Our editor wrote this two-part article explaining why watered-down versions of Medicare for All would not fix our current crisis. This week, Part One:
Readers of Faith in Healthcare know our U.S. healthcare system has big problems. Even though the U.S. continues to spend more per capita on healthcare than any other nation, 27 million U.S. residents are without insurance. Tens of millions more are underinsured. That means millions suffer and tens of thousands even die for lack of care. Here, we go beyond the numbers to share some of the stories of the terrible price our brothers and sisters pay for this shameful state of affairs.
Yet, we may finally be on the brink of real change. “Medicare for All” proposals enjoy an unprecedented level of momentum. Well over half of Americans support a public healthcare system that would cover all people and all costs. They also support that public plan being a single-payer model, thus replacing private insurance companies, provided they can keep access to their preferred providers. That access is a hallmark of Medicare for All legislation that is sponsored by more than 100 members of the U.S. House of Representatives, more than a third of the Democrats in the U.S. Senate, and four leading candidates for President.
Let’s seize this opportunity. And let’s not settle for half-measures that will leave our biggest problem undisturbed.
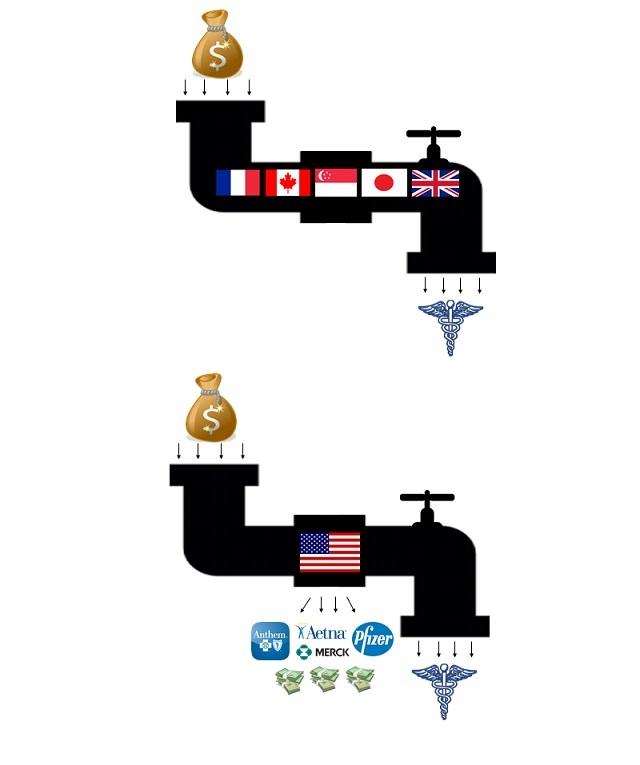
Fixing the Hole in Our Healthcare Pipeline
Despite a significant percentage of Republican voters supporting a Medicare for All program, nearly all of its legislative support comes from within the Democratic Party. Most predictions are that, for the reform to happen, that party will first need to win control over the Presidency and Congress. But it may not be that simple.
Despite the populist demand for momentous change, there are proposals, even within the Democratic Party, that would retain the fundamental flaw of our current, broken system. Senator Joe Biden and several other Presidential candidates support a “public option,” a government health plan that would serve as one choice among existing for-profit private plans. House Speaker Nancy Pelosi supports building on the Affordable Care Act by offering more generous subsidies for purchasing insurance, again from private corporations. And the Democrat-connected think tank Center for American Progress has advanced a proposal called Medicare Extra for All, promising automatic enrollment in health plans. The common thread running through all these proposals is that they allow for-profit insurance corporations to retain their prime spot in the middle of our healthcare system.
So, what’s wrong with that? After all, the ultimate goal for healthcare reform is to ensure universal coverage, not to take down a particular industry. And passing any of these proposals into law would undoubtedly be an easier lift politically than Medicare for All. The health insurance industry already spends tens of millions of dollars on lobbying, political campaign donations, and public relations. Inevitably, the industry will ramp up those efforts to resist a single-payer system that represents an existential threat to its business model.
Yet the proposals from Biden, Pelosi et al. that keep a role for private health insurance are not mere political compromises. They leave undisturbed the fundamental flaw in the U.S. system, the prime reason for the tragic irony of us paying more for worse outcomes than other countries: We waste $500 billion each year in healthcare money spent not on care, but on private insurance corporations’ executive pay, shareholder returns, and a massive bureaucracy devoted to contesting insurance claims and marketing.
The metaphor is an obvious one: other countries enjoy better, less expensive healthcare because they deposit their healthcare dollars into a pipeline that flows directly to patients. In the U.S., we put an historically abundant supply of dollars into the front of our pipeline. But we have allowed a gaping hole to develop in the middle, diverting hundreds of billions in taxpayer dollars to the benefit of wealthy corporate shareholders and CEO’s making as much as $83 million per year . That leaves far too few dollars trickling through to the end of the pipeline, where sick people in need of care are located. If we are going to overhaul our system to finally provide healthcare for all, we need to plug that hole.
Most of the healthcare reform proposals that retain a role for private insurance corporations also preserve at the same time a profound injustice in our current broken system: the deductibles and copays that so often prevent insurance coverage from translating to actual healthcare. Four in ten working Americans have a high-deductible plan that forces them to pay thousands of dollars out of pocket before they get any benefit from the premiums taken from their paychecks each week. The average amount of those deductibles has increased more than 300% in the past decade.
That means that many who are insured are forced to go without care. They skip doctor visits, they don’t fill prescriptions, they cut their pills in half. This is true for many Americans under the current Medicare system, too, with almost 40% of Medicare enrollees reporting that they skip care each year because of cost. The Medicare for All legislation proposals in the U.S. House and Senate use the Medicare name, but they would eliminate co-pays and deductibles. Despite the evidence that patient cost-sharing reduces the care compliance of persons with chronic illnesses, setting those persons up for damaging and expensive health crises, the public option and ACA expansion plans keep those barriers in place.
Taxpayer Healthcare Dollars Funding Huge Corporate Profits, Poor Care
Given the central role that corporate money plays in our U.S. political system, it will come as no surprise that the most fervent supporters of preserving the role of for-profit health insurance corporations are financially tied to . . . for-profit health insurance corporations. Virtually all of the Democratic Party supporters of the public option and ACA expansion receive substantial funding from those corporations.
While well-funded lawmakers and think tanks parrot the industry’s talking points, the industry often takes the messaging into its own hands. Health insurance CEO’s like Cigna’s David Cordani, who has made as much as $49 million in annual compensation, predictably oppose Medicare for All. Instead, Cordani and his colleagues enthusiastically support an expansion of the “public-private partnerships,” arrangements that directly divert taxpayer healthcare dollars to their corporations.
Those partnerships are already substantial. For-profit health insurance corporations received a total of $307 billion in Medicaid dollars in 2018 -- more than half of all state and federal government spending in the program. The Affordable Care Act’s incentives for states to expand Medicaid has caused the number of such arrangements to double in recent years. The corporation Centene, which sells only Medicare, Medicaid and Affordable Care Act plans, made $900 million in profit in 2018.
The basic “managed care” arrangement is that private corporations are paid a set fee from government dollars each month for every Medicaid patient enrolled in their plan. It is not difficult to see the inherent problem here: every dollar that corporations spend on care reduces their profits, and they are in business to make profits. So they achieve savings by restricting patients to a closed network of providers and by denying claims for care reimbursement. “This system is ripe for profit-taking, and there is virtually no penalty for performing badly,” Dr. Andrew Bindman, former director of the federal Agency for Healthcare Research and now a professor at the University of California-San Francisco, told Kaiser Health News in 2018.
In that same report, Kaiser noted that, in California alone, insurance corporations made $5.4 billion in profits from 2014 to 2016. Predictably, a substantial amount of data and reporting shows that some of these private profits came from cutting costs in ways that caused patient suffering. Across multiple states that have outsourced their Medicaid duties to private corporations via the managed care model, lawmakers and patients complain about poorly managed and wrongfully denied care.
For example, in Texas, young D’Ashon Morris was left permanently brain damaged when his Medicaid care was reduced to a dangerously low level. That fateful decision to reduce Morris’ care saved money for the corporation that Texas pays to manage Medicaid, a common enough occurrence that it triggered an award-winning year-long investigation by the Dallas Morning News called “Pain and Profit.” Similar privatizing arrangements have caused an outcry in states like Iowa, where reduced care has led to lawsuits and complaints by both patients and providers.
More broadly, recent research shows that Medicaid members in private corporation plans have more difficulty managing their asthma and blood pressure compared to their counterparts in public programs. Yet the Congressional Budget Office has concluded that pushing Medicaid care to private corporations has actually increased government spending.
Next week, Plug the Profiteering Hole, Part 2: How taxpayers and patients lose with Medicare Advantage plans, the truth about how Americans feel about their for-profit insurance plans, and the problem with a “public option.”
Faith and Healthcare Notes
Most Americans Happy to Switch from Private Plans to Medicare for All A Business Insider poll published earlier this month found that most Americans with employer-sponsored health coverage support switching over to Medicare for All, undermining the right-wing narrative that the U.S. public is wedded to private insurance plans. The survey showed that 59 percent of respondents who have employer-provided insurance said they would "support switching their employer-based health insurance to a government plan under Medicare for All" as long as quality of coverage would remain the same or improve.
Americans with Medicare or Medicaid Like It Better than Those with Private Insurance. The poll also found that Americans on government-run healthcare plans such as Medicare and Medicaid are more satisfied with their coverage than those on employer-sponsored plans, which have soared in cost over the past two decades. According to Business Insider, 57 percent of respondents on government plans said they "love" their coverage, with only 41 percent of those with employer-provided plans saying the same.
Good News: Physician and Med Student Pressure Moves AMA Closer to Medicare for All Support. Also earlier this month, the American Medical Association announced it is dropping out of a coalition called “Partnership for America’s Health Care Future,” a coalition of for-profit insurance, pharmaceutical, and hospital corporations fighting single-payer Medicare for All. The decision comes two months after physicians, nurses, and medical students, along with other activists, demonstrated at the AMA’s annual conference in support of Medicare for All. At the conference, the AMA voted to maintain its resistance to Medicare for All, but with the smallest margin ever: 53% to 47%. That vote, polls showing most medical professionals support Medicare for All, and this new decision by the AMA all suggest that change is on the horizon.
