Why are the same politicians who insist that the U.S. is the greatest nation on earth, including Democrats running for President, also say we are helpless in the face of our healthcare crisis? With every other economically advanced nation managing to run a universal healthcare system, are we really that much less capable than Taiwan or Switzerland or Australia?
Of course not.
What is true is that our current healthcare access performance is bottom-of-the-barrel. The Commonwealth Fund’s most recent study of 11 wealthy nations shows the U.S. somehow pulling off the shameful feat of having both the most expensive healthcare system yet the worst outcomes, equity, care delivery, and administrative efficiency. One-third of Americans reported skipping medicines or care due to cost, a rate more than four times any of the other countries surveyed.
Ugh.
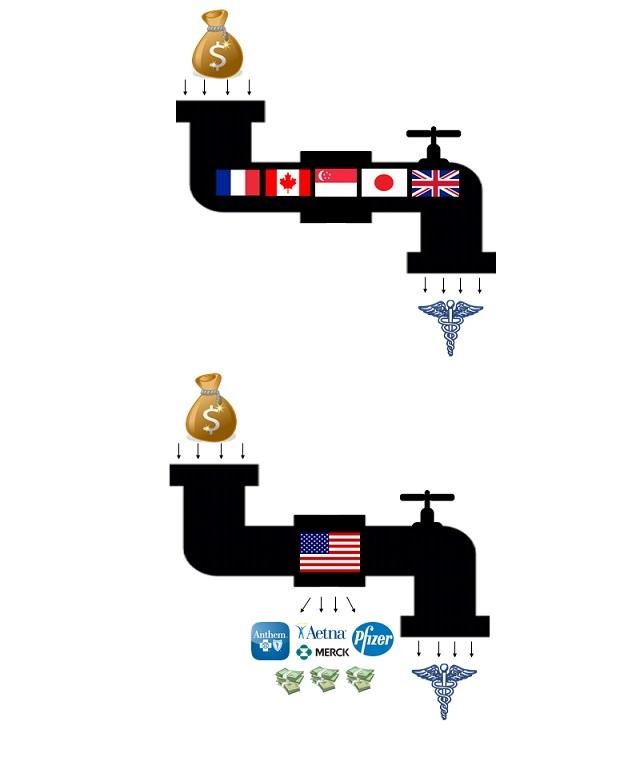
But it doesn’t have to be this way. The silver lining in our currently dismal state is that we have a lot of models to learn from where other nations have done far better for far less. As discussed previously in Faith in Healthcare (“Plugging the Profiteering Hole in our Healthcare System”), the common denominator among those nations is that they refuse to allow corporations to make billions and executives to make tens of millions off of relentless price-gouging of sick people.
Yet those nations do follow different paths on their way to more just, affordable outcomes. Reviewing a few of the options is a useful exercise for the U.S. as we contemplate change, in part because it exposes the lie that we can’t afford to do better:
Socialized Medicine: Fear-mongering rhetoric aside, U.S. proposals for Medicare for All, which would retain private providers and institutions, are not socialized medicine. But the U.K. system is. The National Health Service pays for care via tax revenues, not private insurance, and often provides it directly as well. Most hospitals and clinics are operated by the government, and care policies and payment rates are determined at the national level.
Like most nations, the U.K. also has a small privately-funded system running parallel to the government one. But nearly everyone is cared for in a government setting and often by a government employee, similar to the U.S. Veterans Administration model. Patients are seen quickly, and not shut out of care due to inability to pay an insurance premium or co-pay: the Commonwealth Fund analysis ranked the U.K. tops in access to care, administrative efficiency.
Single-Payer: Many in the U.S. are aware of the Canadian single-payer system, where the government is the only entity paying medical costs, and everyone is enrolled in the same plan. Australia and Taiwan are among other nations with similar approaches. Unlike the U.K. system, providers are not government employees. These countries’ residents possess a card that gives them access to whatever private provider they choose, with those providers billing the government for the care.
Taiwan provides an interesting model in part because they created it recently, in 1995, after studying the other care systems in place across the world. Single-payer systems’ removal of private insurance from the process helps keep their administrative costs quite low, compared to the U.S. level that is estimated to be as high as 30%. The U.S. Medicare system operates in a similar way, and most Medicare for All proposals in the U.S. are single-payer models.
Government-Subsidized Non-Profit Health Insurance. Some healthcare analysts, mindful of the U.S. preference for individual control and choice in healthcare, say that the best model for the U.S. to follow would be the “multi-payer” systems in nations like Germany, Japan, France, and Switzerland. Like in the U.S., most persons in those countries sign up for health care through an insurance provider that is independent from the government.
But, unlike in the U.S. model, these insurance companies are non-profit, and their rates and coverage are very tightly regulated by the government. In a weighted debate among healthcare experts conducted by the New York Times in 2017, multi-payer systems Germany and Switzerland were preferred.
The U.S. does not have to mimic any of these nations, but we absolutely can learn from them. They show us that we have the ability to take our record-high dollars spent on healthcare and put them to good use, ensuring care for all at an affordable cost.
Faith and Healthcare Notes
One of every eight Americans had a friend or family member die because of not affording medicines or treatment. A new study by Gallup and West Health shows that more than 13% of American adults -- 34 million people -- report knowing of at least one friend or family member in the past five years who died after not receiving needed medical treatment because they were unable to pay for it.
Economic struggles already leading to millennial health problems. BlueCross BlueShield reports that millennials are already experiencing greater financial hardship and significantly poorer health than the generation preceding them, fueled in part by lack of access to care and economic pressures like low-wage work and student loan debt.
Healthcare is the top issue in states expected to decide the 2020 Presidential election. The Kaiser Family Foundation and Cook Political Report polling shows that healthcare is the top issue for voters in so-called “battleground” states, with healthcare also being the category where President Trump receives his lowest marks.
